Autopsy evidence that fetal asphyxia can occur before labor
After all of the autopsy evidence on a stillborn infant is finally gathered, there may be a profound disappointment in that there is no answer. Nothing really explains the death of this normally formed, normally grown infant from an uncomplicated pregnancy. Still, there are clues, often subtle anatomic findings, that potentially tell us something about the mechanism of death. The pathologist has two ways to extract meaning from the findings. One way is the time tested approach of comparing the findings in a known cause of stillbirth with those in an unknown cause. The other is to compare the findings with those in experimental causes of fetal death or at least the anticipated findings had the animals been autopsied in detail.
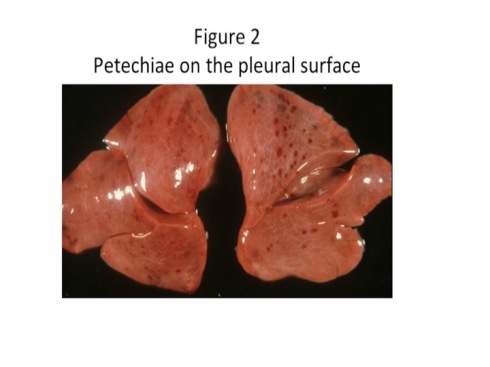
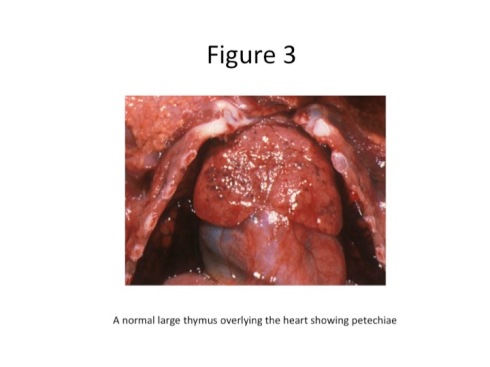
Using the first approach, I have compared the findings in fetal death from premature placental separation between those in which the placenta appears suddenly, and totally, or almost totally, separated from the uterine wall with placentas showing lesser degrees of separation1. The first group is the equivalent of sudden acute asphyxia usually achieved experimentally by clamping the umbilical cord or the maternal uterine arteries. Fetal respiration comes to a sudden stop. The second group resembles models of partial asphyxia with a decrease in oxygenation and a gradual increase in metabolic, mostly lactic, acidosis. The first group showed more aspirated squames (the shed skin surface cells that accumulate as vernix in the amniotic fluid) in the lungs (Fig 1). If meconium was present they also demonstrated more aspiration of that mix of squames and pigmented protein. (Passage of meconium into the amniotic fluid will be discussed in a later section.) They also demonstrated petechiae (dot like hemorrhages) on the surfaces of the organs in the thorax, namely the thymus, pleura of the lungs, and epicardial surface of the heart (Fig 2,3).
Figure 1
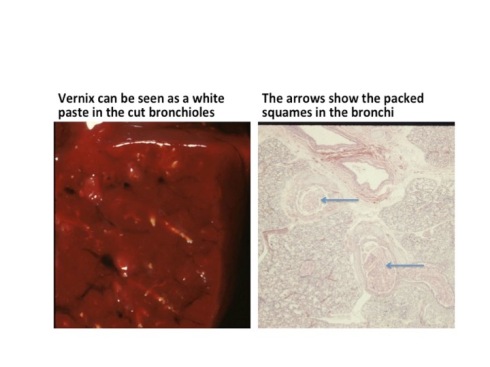
We have already seen that acute asphyxia induces violent gasping which would explain the aspirated material in the lungs since the fetus is gasping within the vernix filled amniotic fluid. As a practical matter, there is some interpretation involved in evaluating the microscopic evidence. Normal shallow fetal respiration does seem to mix a limited number of squames into the airway, but the asphyxiated fetuses often pack or even distend their airways with the debris. The amount of vernix increases with gestation and would not accumulate in large amounts at younger gestation. The vernix may have settled away from the fetal mouth at the time of gasping if the mother had been at rest. Not finding airways packed with squames does not exclude asphyxial gasping, but finding them certainly is evidence that the fetus suffered acute asphyxia.
The explanation of the petechiae has the same significance as a marker of gasping, but the path of reasoning is much less direct. Petechial hemorrhages occur when a distended capillary ruptures. The rupture likely occurs where the capillary is deformed like a small aneurysm on its least supported surface. A classic test for scurvy, vitamin C deficiency that weakens the collagen encircling the capillary, was to inflate a blood pressure cuff on the arm at a pressure that let arterial blood in, but blocked blood flow out of the arm. The capillaries would overfill and burst on the skin surface if scurvy had weakened them. There are other causes of petechial hemorrhages, but keep the image of this mechanism mind, as we pursue further evidence.
A similar pattern of intrathoracic petechiae is a common feature in the autopsy of infants with Sudden Infant Death Syndrome (SIDS)2,3. One explanation for the petechiae follows from the understanding that some SIDS occurs with the infant in the prone position. In this position if a blanket or other deformable surface is against the nose and mouth of the infant, the infant can exhale pushing the surface away, but inhaling will be blocked by the surface sucking upward. Thus, the lungs become emptied to their residual volume by exhalation, at the same time that the infant is gasping to maximally expand the chest. The combination of the deflated lungs and expanded chest would create a large vacuum or negative pressure in the chest cavity. This in effect would suck blood into the lungs distending the capillaries, and the negative pressure in the chest cavity would distort the surface capillaries that did not have strong surrounding tissue support. As a result, these aneursymally dilated, over-distended capillaries would rupture. At least in SIDS, the lack of petechiae in the cervical portion of the thymus is in keeping with this explanation.
Some years ago we had Dr. Bruce Beckwith, an expert on SIDS pathology, as guest faculty, and he explained that the above scenario corresponds with the experimental production of intrathoracic petechiae. If an animal’s trachea is occluded at end expiration, intrathoacic petechiae occur, but if the trachea is occluded at other points in the respiratory cycle when the lungs have more air, the petechiae are inhibited. While this is all very important to understanding SIDS, how does it relate to stillbirth?
To start, the fetal lungs which are fluid filled are equivalent in volume to end expiratory volume because they are not expanded with air. Second, acute asphyxia causes marked gasping respiration. The only point missing from this analogy with SIDS is the occluded airway. This requires a leap of faith, but it is possible that the fluid filled pharynx initially occludes inspiration. In utero the accumulation of squames suggests that the occluded airway does eventually open although the lung does not markedly expand with amniotic fluid likely because of the intra-amniotic pressure, lack of a surfactant coated air interface and perhaps higher resistance of liquid movement. I do not know if an infant taking a normal first breath develops intrathoracic petechiae because almost all infants dying immediately after normal respiration have other complicating factors such a pulmonary hypoplasia or shock with petechiae in many organs.
A reasonable argument is that intrathoracic petechiae that are not in the context of shock with disseminated intravascular coagulation and diffuse petechiae, are evidence of gasping most likely in response to acute asphyxia. This is confirmed by the lack of such petechiae in the cases of partial separation that would be expected to become acidotic and apneic over a longer period of time. Equally confirmatory is that intrathoracic petechiae are present in other known causes of intrauterine acute asphyxia.
This gets us part way to a solution. These unexplained deaths died from acute complete asphyxia. These cases by definition had no anatomic cause of death, for example exsanguination, hydrops, shock, infection, etc. and no obvious maternal complications such as cardiac arrest or respiratory failure. While a very acute complete premature placental separation can be impossible to detect in the placenta, there is usually a clinical history of placental abruption. Conceivably severe uterine tetany could be overlooked long enough to cause fetal death, but that also seems very unlikely. By exclusion, the most likely explanation of these deaths involves an occlusion of the fetal circulation most likely in the umbilical cord, although cardiac asystole is conceivable.
Some of the next sections will consider how the umbilical cord can or could be compromised.
References:
- Bendon RW. Review of autopsies of stillborn infants with retroplacental hematoma or hemorrhage. Pediatr Dev Pathol 2011;14:10-5.
- Krous HF. The microscopic distribution of intrathoracic petechiae in sudden infant death syndrome. Arch Pathol Lab Med 1984;108:77-9.
- Beckwith JB. Intrathoracic petechial hemorrhages: a clue to the mechanism of death in sudden infant death syndrome. Biol Psych 1990;28:37-47.